Live your best to life’s end.
There’s still lots of life to live–whatever health and medical decisions that may be ahead. For many, feeling ‘alive’ right to the end means feeling useful for as long as possible. For others, it’s peace of mind that brings a peaceful end. For most, it’s feeling wanted, valued, respected and listened-to that are all-important. The pleasures of everyday life can be just as meaningful: what makes you smile, what brings you happiness and joy and what gives you comfort.
It’s often that small stuff that can make a big difference: There are creative ways to accomplish what may seem out of reach – like the man on the rock who may not be able to be physically near an ocean, but may be able to turn to technology to inspire a solution. Paying attention to small pleasures shifts the focus from ‘what I don’t want at life’s end’ to ‘what will make a positive difference to me at life’s end.’ It’s an approach with its own reward: helping someone have the best end can help everyone involved.
Need Inspiration?
How would you fill in the blank? Check out whiteboards and 60-second BestEndings videos: instagram @MyBestEndings
Need Information?
It can be a long road to learning about and planning for the best end-of-life experience. There’s lots to consider and emotions to tackle. Pick your own starting points: personal or medical decisions or specific topics. You can come back for more and then document your end of life wishes
Caring for aging parents: Chronic illness
Heart and kidney failure, frailty, Alzheimer’s, Lung Disease, Diabetes
Palliative Comfort Care and Quality of Life
The Palliative and Hospice approach: comfort and quality of life is what it’s all about
Understanding Medical Terms and Jargon
Cardio Pulmonary Resuscitation: CPR, Do Not Resuscitate: DNR, Allow Natural Death: A.N.D
Traditions, Culture and Being Remembered
Time honored customs can help at life’s end, ways to keep memories alive.
Modern Medicine can keep you alive
End of life: grief and bereavement
Knowing what End of Life looks like can ease the process; often grief starts long before the end.
Decision-Makers: Consent and Conflict
Surrogate, Substitute, Agent, Proxy: who will make sure your end of life wishes are followed.
Advance Directives, Living Will, End of Life Wishes
Create your own end of life, Advance Directives Living Will with an interactive form
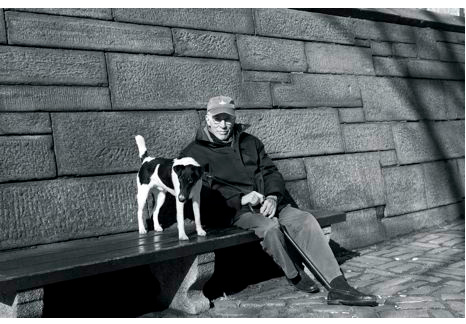
Men writing about The End of Life
Men writing from the inside out about life’s end. In the picture in The New Yorker, sitting with his dog, on a bench by a park, Roger Angell, looked none of his 93 years. Famous for his sports writing, ‘This Old Man' is Angell's reflection on life, starting ith what...

Palliative Care: Doing ‘nothing’ is not an option
Dr Daphna Grossman wants to set the record straight “In healthcare it seems we talk about ‘doing everything’ or ‘doing nothing’. With Palliative care ‘nothing’ is not an option.

Infections in the elderly how to best treat: Are antibiotics always the answer
Although my 96 year old aunt (pictured at left, between me and my cousin – her daughter) had no symptoms of a bladder infection, a urine test resulting from cloudy pee revealed she indeed had a Urinary Tract Infection (UTI. My aunt hadn’t complained about pain or discomfort, my cousin – her ‘power of attorney’ – authorized treatment with antibiotics. Many would agree.
Room 217: Care Through Music
Guest blog by Bev Foster A lot of life happens in rooms and so does a lot of death. One room I will always remember is Room 217, where my mom, five siblings, and I sang around dad’s bedside as he was dying in a hospital northeast of Toronto. Whether it was the...
As we age, do we become too thin-skinned?
In a word: Yep. Our skin thins and gets dry Thin, dry skin often gets itchy. And that can lead to a mess of problems. Hence, the expression: thin-skinned. Perhaps not as talked about as the other issues of aging, but should be – considering how much skin we have. Dr...
Medications: work differently and more dangerously as we age
Drug Use and Seniors 1 in 5 over age 65 are taking 10 or more prescription medications, 1 in 20 are taking 15 more so reports Canadian Institute of Health Information (CIHI). Not included in that total: the number of times a day meds are taken and non-prescription...
Coalition for Compassionate Care Summit with ePatients
ePatients: Engaged and Empowered and Invited The Coalition for Compassionate Care of California (CCCC) promotes high-quality, compassionate care for everyone who is seriously ill or nearing the end of life. What a human-centered, patient-centered goal. And now,...
Advance Care Planning: Women’s College Hospital and Kathy Kastner
National Advance Care Planning Day sees Women's College Hospital as leaders: bringing the first consumer-created End-of-Life website to Family Doctors. TORONTO APRIL 16...Women's College Hospital (WCH) is the first to embark on a project with Family Doctors and...

Palliative Home Visits are the Future
“What I fear the most – what really terrifies me – is being short of breath and not being able to swallow.” So said the husband of his dying wife. This is terrifying to me, too, so I listened closely to the response given by Palliative Care physician, Dr Sandy...