Medical Terminology
Medical Terminology
Every health condition comes with its own language, medical terminology and decision options. End of Life is no different. While CPR and DNR may be familiar to many, that doesn’t mean they are understood as intended.
New ‘terms’ such as Allow Natural Death or AND and Voluntary Stopping Eating and Drinking or VSED have been created to add to options to consider. Understanding the words and terms used is one thing. Being able to act on them is another.
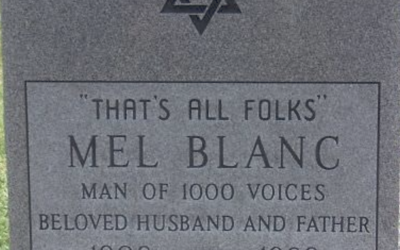
To Tombstone or not to Tombstone
I don’t know where my parents are buried. I was at both their burials, in different graveyards. I don’t remember where. Nor do their graves have headstones. Many find this weird, even off-putting. I don’t miss having a grave or headstone to commemorate.I don’t...
Medical Aid in Dying: I signed up to be a witness
I was nervous about this new role I’d signed up for: volunteering to be one of two witnesses to make official a patient’s request for medical assistance in dying.This involves witnessing the paperwork necessary for a MAID (Medical Aid in Dying) request. The...
Live in memory, Live in love
This is Sam, my father-in-law. He's going into his 103 year, and is still smiling. Yet every night, his last words before falling asleep: God, please let me die He's not suffering in any major way: the swollen ankles and chronically congested chest don't bother him...
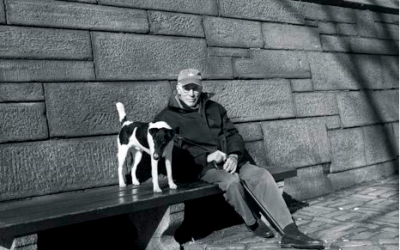
Men writing about The End of Life
Men writing from the inside out about life’s end. In the picture in The New Yorker, sitting with his dog, on a bench by a park, Roger Angell, looked none of his 93 years. Famous for his sports writing, ‘This Old Man' is Angell's reflection on life, starting ith what...