by KathyKastner | Mar 23, 2025 | Blog, Inspiration
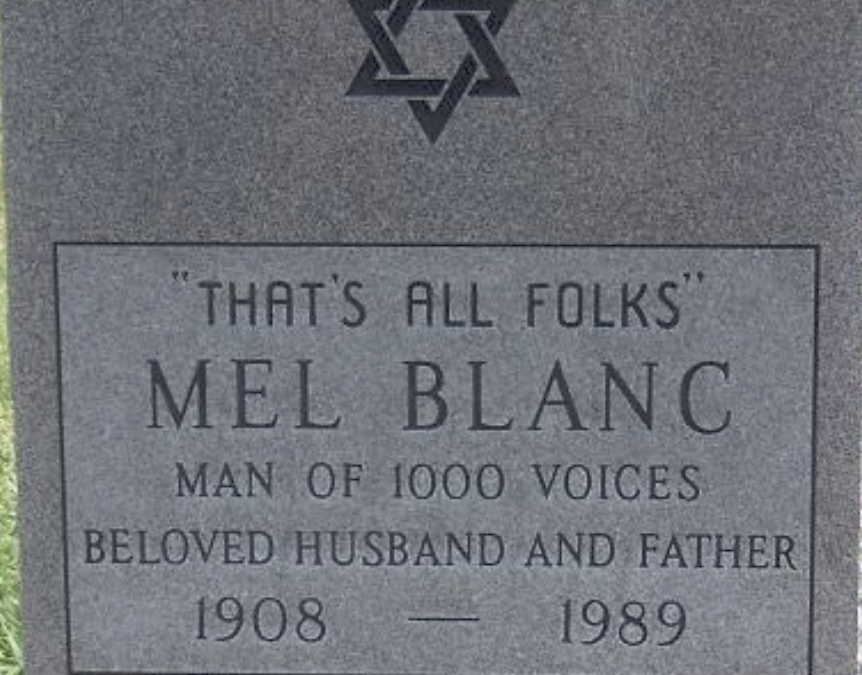
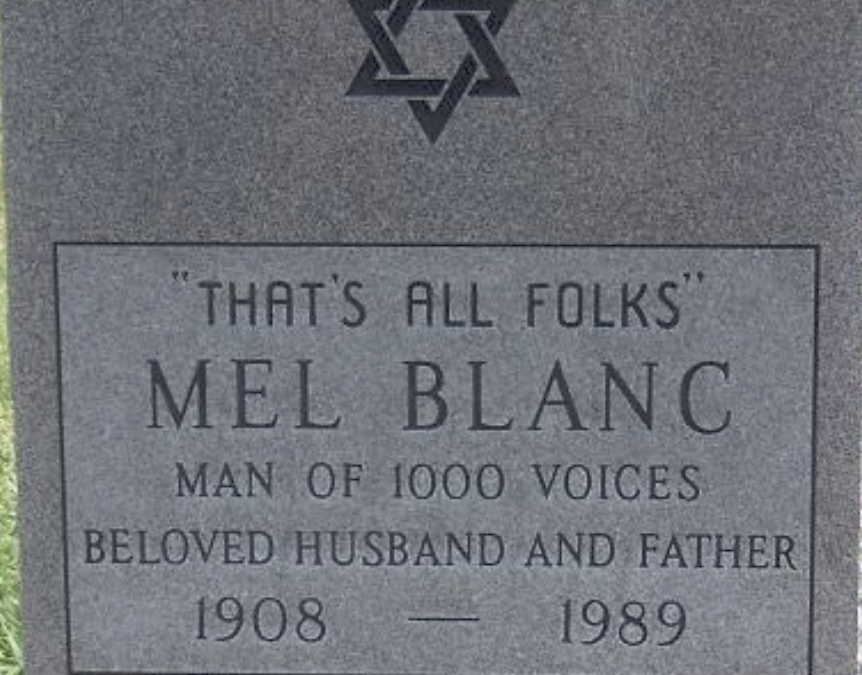
I don’t know where my parents are buried. I was at both their burials, in different graveyards. I don’t remember where. Nor do their graves have headstones. Many find this weird, even off-putting. I don’t miss having a grave or headstone to commemorate.I don’t...

by KathyKastner | Jan 27, 2024 | Blog, Featured
I was nervous about this new role I’d signed up for: volunteering to be one of two witnesses to make official a patient’s request for medical assistance in dying.This involves witnessing the paperwork necessary for a MAID (Medical Aid in Dying) request. The...

by KathyKastner | Mar 17, 2023 | Blog, Featured
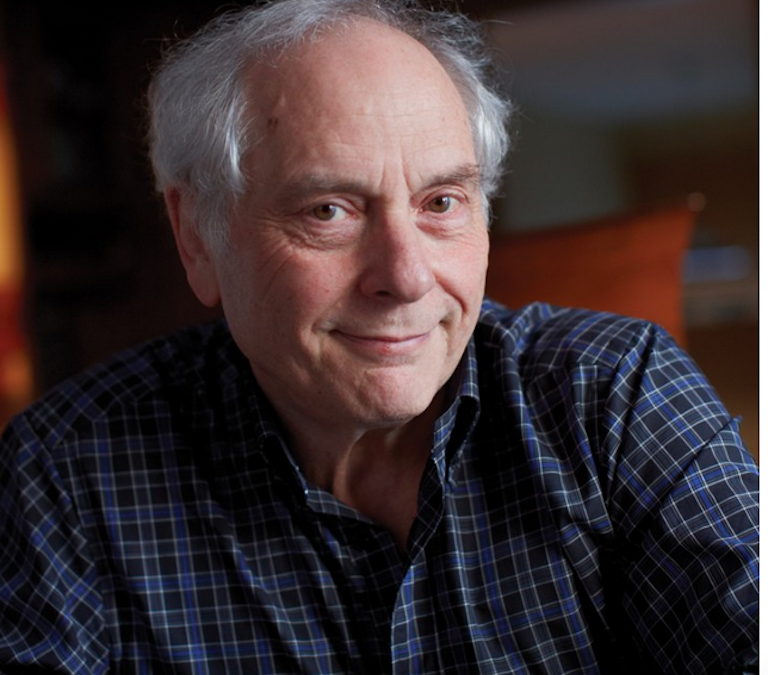
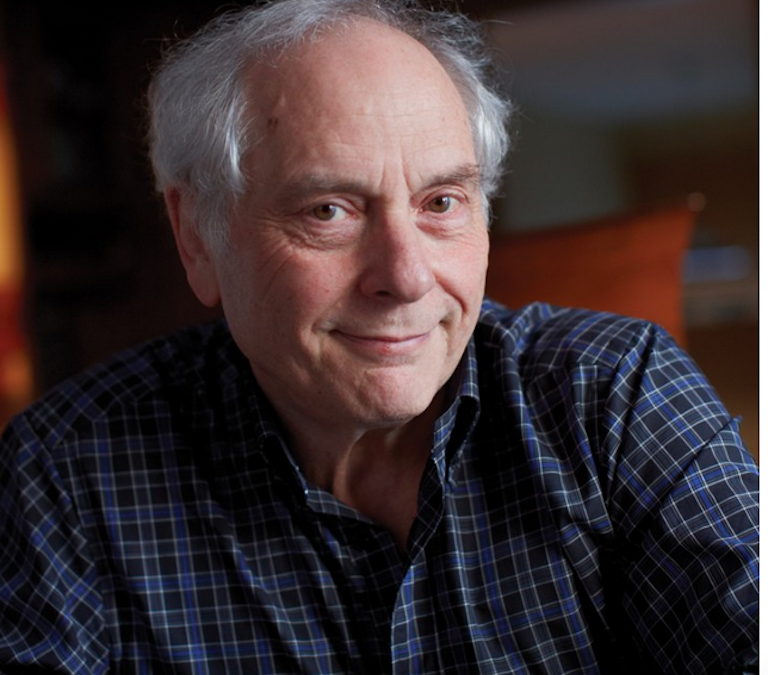
This is Sam, my father-in-law. He’s going into his 103 year, and is still smiling. Yet every night, his last words before falling asleep: God, please let me die He’s not suffering in any major way: the swollen ankles and chronically congested chest...
by KathyKastner | Dec 30, 2019 | Personal Stories
My bro died at home, on Palliative/Hospice Care Although we did not know it at the time, my brother’s ‘end’ started November 2018, with a brain tumour diagnosis. Surgery before Christmas that year was deemed ‘successful’ and John was in...
by KathyKastner | Feb 25, 2019 | Blog
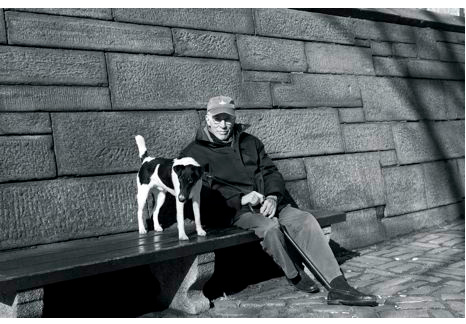
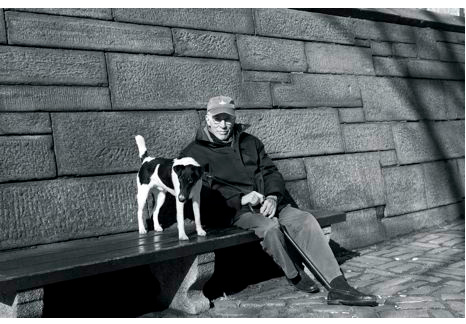
Men writing from the inside out about life’s end. In the picture in The New Yorker, sitting with his dog, on a bench by a park, Roger Angell, looked none of his 93 years. Famous for his sports writing, ‘This Old Man’ is Angell’s reflection on life,...