by KathyKastner | Mar 23, 2025 | Blog, Inspiration
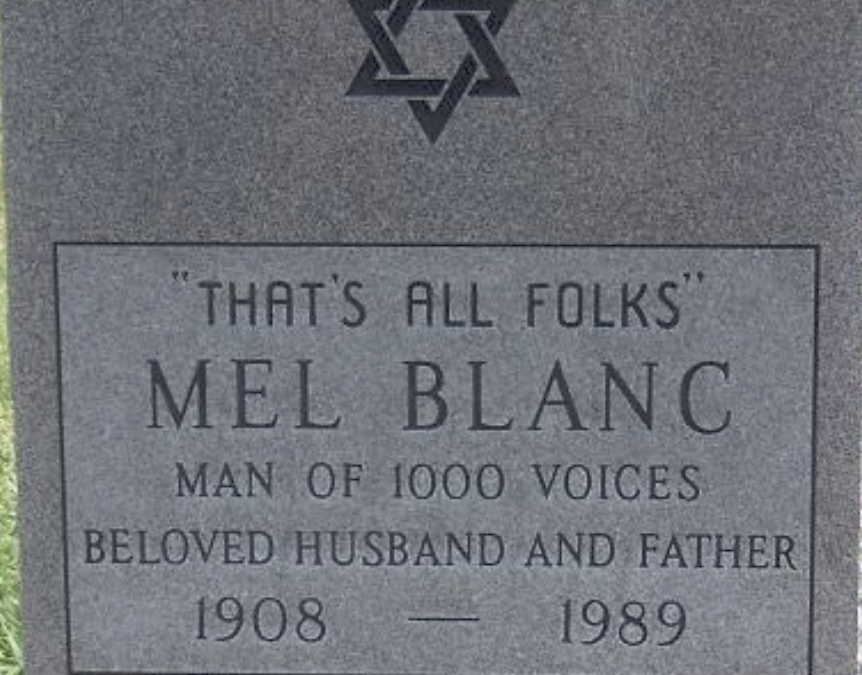
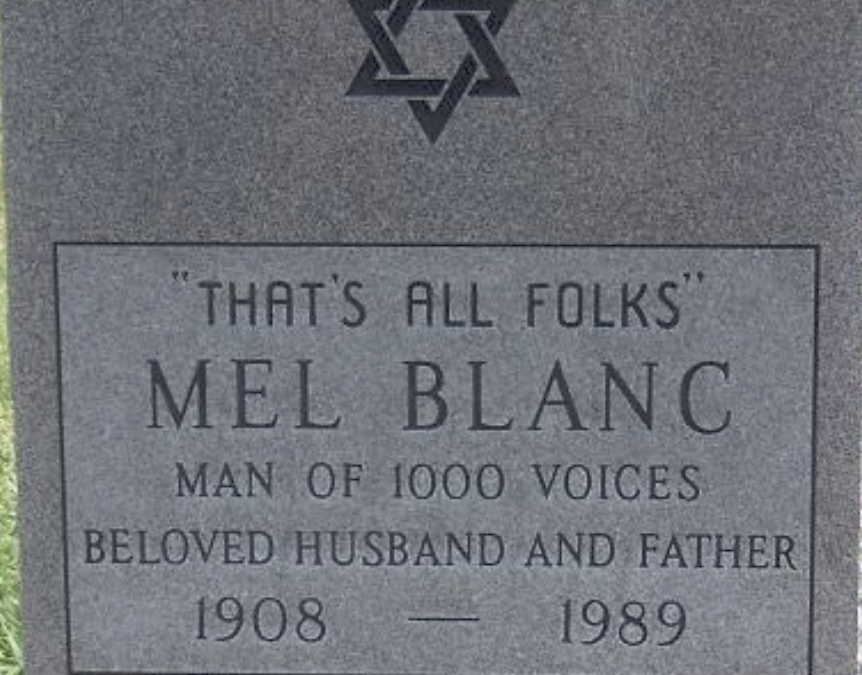
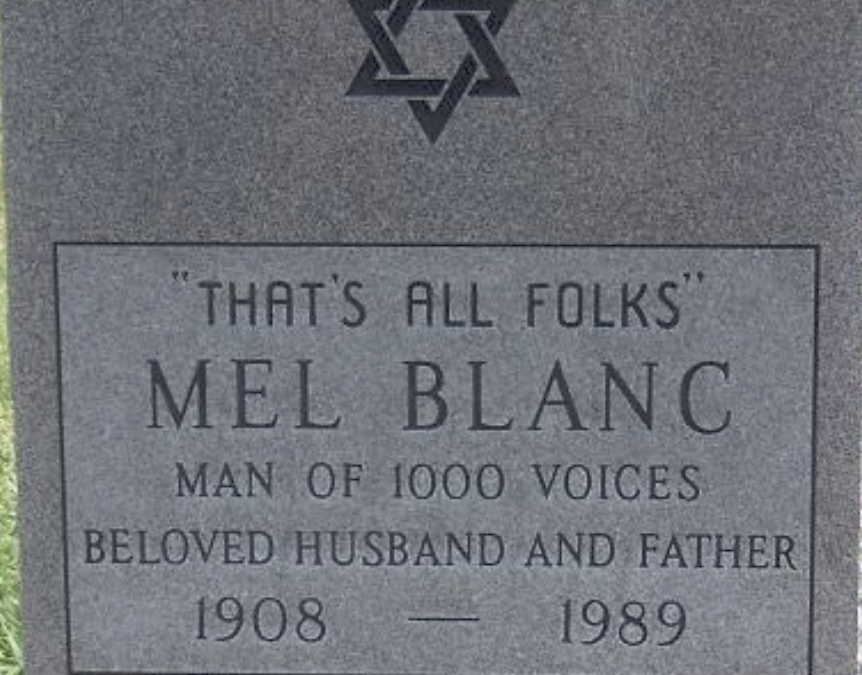
I don’t know where my parents are buried. I was at both their burials, in different graveyards. I don’t remember where. Nor do their graves have headstones. Many find this weird, even off-putting. I don’t miss having a grave or headstone to commemorate.I don’t...

by KathyKastner | Jan 27, 2024 | Blog, Featured
I was nervous about this new role I’d signed up for: volunteering to be one of two witnesses to make official a patient’s request for medical assistance in dying.This involves witnessing the paperwork necessary for a MAID (Medical Aid in Dying) request. The...

by KathyKastner | Mar 17, 2023 | Blog, Featured
This is Sam, my father-in-law. He’s going into his 103 year, and is still smiling. Yet every night, his last words before falling asleep: God, please let me die He’s not suffering in any major way: the swollen ankles and chronically congested chest...
by KathyKastner | Feb 25, 2019 | Blog
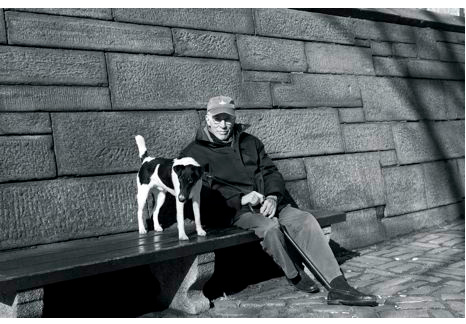
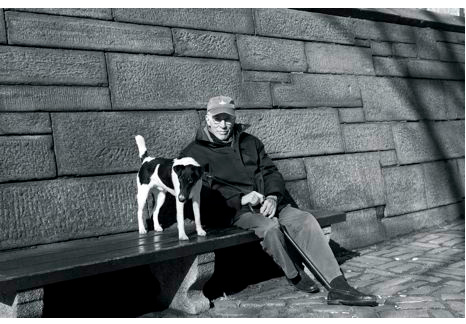
Men writing from the inside out about life’s end. In the picture in The New Yorker, sitting with his dog, on a bench by a park, Roger Angell, looked none of his 93 years. Famous for his sports writing, ‘This Old Man’ is Angell’s reflection on life,...

by KathyKastner | Jul 27, 2018 | Blog, Kathy Kastner
Dr Daphna Grossman wants to set the record straight “In healthcare it seems we talk about ‘doing everything’ or ‘doing nothing’. With Palliative care ‘nothing’ is not an option. Certainly there are standards and recommendations and then there’s the Art of Treatment:...

by KathyKastner | Jun 21, 2018 | Blog, Medical Decisions
‘If you don’t give her antibiotics, she’ll go toxic and die.” Although my 96 year old aunt (pictured at left, between me and my cousin – her daughter) had no symptoms of a bladder infection, a urine test resulting from cloudy pee revealed she indeed had a...