by KathyKastner | Mar 23, 2025 | Blog, Inspiration
I don’t know where my parents are buried. I was at both their burials, in different graveyards. I don’t remember where. Nor do their graves have headstones. Many find this weird, even off-putting. I don’t miss having a grave or headstone to commemorate.I don’t...
by KathyKastner | Oct 14, 2015 | Blog, Inspiration
It was a day of music, arts and drama, of passion and compassion, entitled, Bringing Creativity into Clinical Practice with older adults. Bringing creativity into a Clinic Day brought relief and hope to many working with Dementia and Alzheimer’s patients. The...
by KathyKastner | Oct 5, 2015 | Blog, Inspiration
“I’m 62. I was diagnosed at 46. You do the math” Christine Bryden, Person with Dementia 16 years of living with Alzheimer’s and Christine Bryden’s making the audience of 300 laugh and cry at A Changing Melody: A learning and sharing forum for persons with Early Stage...
by KathyKastner | Aug 9, 2015 | Blog, Inspiration, Personal Stories
Dealing with grief and End of Life as a Personal Support Worker Guest Post by Natrice Rese It’s something that you are prepared for as a student. It is understood that as a caregiver, a PSW, you will maintain a distance, a separation, a formal kind of...
by KathyKastner | Jul 25, 2015 | Blog, Inspiration, Kathy Kastner
With Mary Ito, host of FreshAir: celebrating after our interview on CBC Radio about what this ‘layman’ brings to conversations about end of life Click to listen: 11 minutes...
by KathyKastner | Jul 22, 2015 | Blog, Inspiration, Personal Decisions
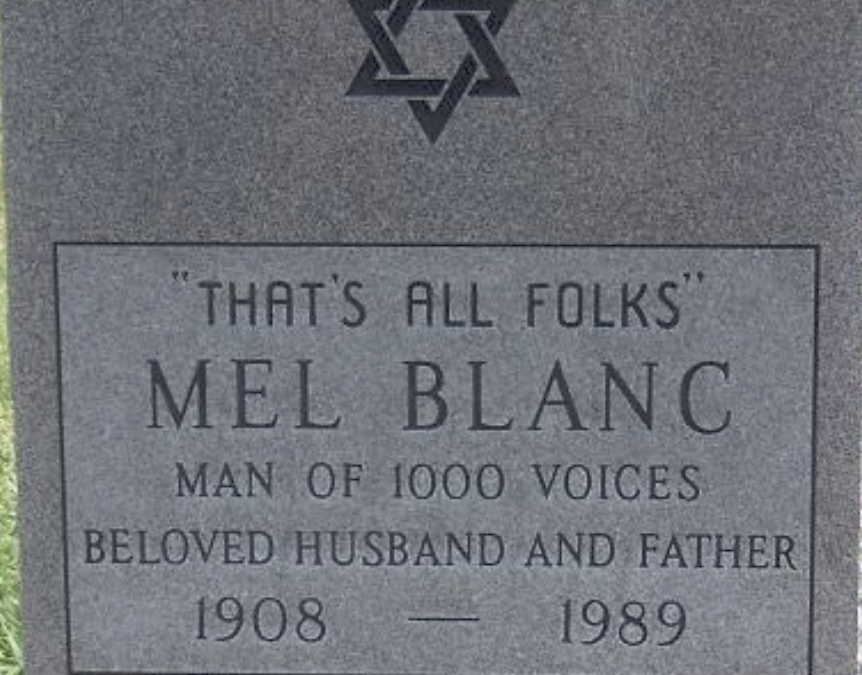
I’m noticing new approaches to obituaries Defying a history of somber and factual, I’m seeing welcomed injections of humour – including obits written by the deceased. Before, of course. This means leaving blanks as you can see from above picture....