ePatients: Engaged and Empowered and Invited
What a human-centered, patient-centered goal. And now, the Coalition includes the patient’s point of view – their first Summit with ePatients : we who are not afraid to look beyond, ask beyond and search beyond what we’ve heard in doctor’s offices. It’s a given that the ‘e’ includes electronic (email, forums, searches) connectivity after all, in between doctor’s visits patients live their lives, and turn to the digital world for support comfort and information.
Palliative approach: ripe for ‘ePatient engagement’
Since Palliative care focuses on all aspects of comfort (or as palliative doc, Daphna Grossman put it: doing ‘Nothing’ is not an option) patients and families have ample time to learn about what may be ahead, and put put mind to what’s important long before the end may seem nigh. Comfort itself can mean many things, in addition to the all-important pain management. The palliative approach: perfect opportunity for ‘engagement’.
ePatient: Educate and Encourage and Evangelize about Palliative Care
Great keynote by #ePatientdave with @KathyKastner in foreground at #cccc16! pic.twitter.com/XEOcpm39ir
— Elizabeth Bailey (@PatientPOV) May 12, 2016
This is one of the many reasons I was so over-the-moon at the decision to invite patients to the Summit, and was even more so when I was selected. This, especially so because my fellow ePatients are living with chronic conditions – whether themselves or those they care for – where I am not. Rather I am immersed in the crises, the nuances and the decisions as life winds down. I consider myself an ePatient Educator and Encourage-r and for sure another ‘e’: Palliative Care Evangelist
Even for the most involved ePatients, such as Keynote-er kidney cancer survivor and dedicated ePatient Dave deBronkart (@ePatientDave) end of life often starts and stops with to prolong or not to prolong, whilst not being fully informed on what that might entail. We had a conversation about end-of-life issues when Dave and I dined together after a Patients2.0 presentation I was part of.
Dave said: “I’ve told my wife, if I lose my mind just let me go.”
Said I to Dave: ‘there is much more to think about, make and direct decisions about than ‘just let me go’. Who knows but it may be that your wife wants a say in the matter.’
End of life health decisions are rarely made in isolation
CCCC CEO, Judy Thomas made the point that health decisions aren’t made in isolation.
“We don’t make health decisions by ourselves” TY @JudyThomasJD -> rarely gets acknowledged yet critical in #endoflife convos #hpm #cccc16
— kathy kastner (@KathyKastner) May 12, 2016
As beautifully and heartbreakingly told in her Keynote, Katy Butler, journalist and author of Knocking on Heaven’s Door, end of life medical decisions are often influenced by forces that don’t represent the most beneficial patient choices such as when doctors insist on procedures that solve a problem that the patient doesn’t want solved.
The pacemaker solved a “problem that was not a problem for our family, but a problem for the cardiologist” @KatyButlerHeart story at #cccc16
— Amber E. Barnato MD (@abarnato) May 13, 2016
In addition to the ab fab keynotes, there were excellent breakout sessions. CCCC Medical Director of Consulting Services, Dr Lael Duncan shared insights, encouragement and suggestions to fellow professionals on the topic of ‘difficult conversations with seriously sick patients.’
‘You will make people.. sad/frightened… forgive yourself in advance for anything that happens. Let go of outcome -> @lduncanMS #cccc16
— kathy kastner (@KathyKastner) May 13, 2016
As always, my hottest button is in the communication gaps and de-humanizing language, so was pleased to hear there’s increasing sensitivity:
friendly language: ‘At Kaiser, we never use ‘futile’ we use ‘non-beneficial’ Pls change ‘withhold treatment’ to ‘not start’ #cccc16
— kathy kastner (@KathyKastner) May 13, 2016
From conversations about the emotional impact of having conversations with patients about life’s end, I see the stresses of the system working against healthcare professionals ability to see things from our point of view, So, when I stood, with some trepidation, and was warmly greeted:
Patients are strangers in a strange land @KathyKastner How true! #cccc16
— Judy (Citko) Thomas (@JudyThomasJD) May 13, 2016
Later, I saw the tweet about making language of healthcare professionals more patient-friendly: re-wording ‘advancing illness’. and ‘goals of care’ and Not so hard to do, I thought:
How bout: ‘getting worse’, ‘what are you hoping for’ MT @Robert_Moore_MD: translate: advanced, progress, prognosis, goals of care. #cccc16
— kathy kastner (@KathyKastner) May 13, 2016
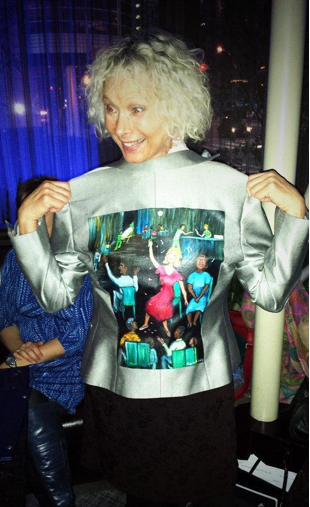
This post is dedicate to my mother: an early ePatient long before the internet changed the world. She researched at the library and sent old fashioned letters in the hope of recognition when doctors refused to believe she had Hemophilia (rare in women). It’s my mother dancing in red that’s on my treasured WalkingGalleryJacket, painted by fellow ePatient Regina Holliday.