
What makes us want to live, and at what cost?
“Do not go gentle into that good night”
So wrote Dylan Thomas, in his battle cry about fighting death. He lived in a time before medicine and medical advancements have enabled us to live so much longer. Having been given more years, we each have our own perception of life and its quality.
We may be dying for different reasons than 100 years ago and we may be dying differently, but we still have the same human instincts as life winds down:
Dying is about finishing up the “unfinished business” of one’s life and preparing for what’s to come. Family members may need to express long held back feelings. Time is sometimes so short that family members may not have had time to even travel to be at their loved one’s side. If family members live in different States or even countries, distance becomes a great obstacle to family members who wish to be at the bedside at the time of death.” From the Journal of Medical Ethics:
Those who work with the dying witness – and marvel – time and again the will to live for a certain milestone be it a birthday or holiday:
Father Michel Malloy, rector at Our Lady of Perpetual Help Cathedral in Rapid City, said in his 36 years as a priest, he has seen numerous instances in which the will to live carries his congregants to a milestone.
“I have seen times when people have lived to a certain point that is connected to a major event in their life,” Malloy said. “From my experience, that’s what they waited for. When that day arrived, they decided not to fight anymore.” rapidcityjournal.com
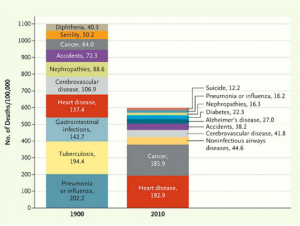 |
From the magazine, The Atlantic: A historical perspective of what we died of then.. and now |
Quality of Life or What kind of life is that?
Having been given more years, we each have our own idea of life and its quality.In the medical world, the term ‘futile’ is often used to assess the benefits of any given intervention. The perception and interpretation of ‘futile’ is often quite different for the patient and family, than for the health care professionals:
After their 89-year old father suffered a stroke and developed Sepsis (a whole body infection) doctors encouraged a DNR (do not resuscitate) along with palliative care. Although advised that Sepsis can cause lasting damage, he and his sister were in agreement: keep Dad alive. Sepsis was treated but took it’s toll: Dad was left without speech, paralyzed on his left side and with Dementia. For he and his sis, there was no question it was the right decision:
“No DNR: our father’s a Holocaust survivor. He’s a fighter. He wants to live. Dad smiles, loves hugs and his happy to see us. True, he can’t speak but we find ways to communicate. We’re happy.”
When planning your Advance Directives, using the BestEndings, tool, consider which interventions you may want to have to prolong life.
Interesting reading: End of Life Machinery:the good and the bad